Treatment planning and automation
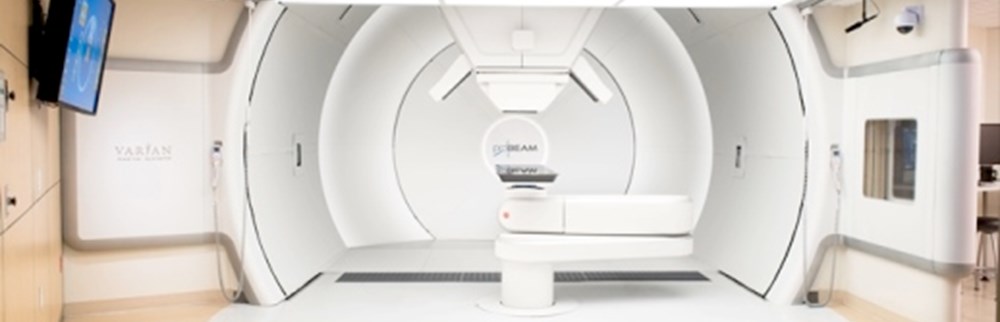
New treatment modalities like proton therapy at the Danish Center for Particle Therapy and on-line MRI-guided radiotherapy at Copenhagen and Odense University Hospitals are introduced in the coming years. In this project, a national initiative for standards and automation will support the development and dissemination of best practices and support national protocols for clinical research and selection of patients for the new treatment modalities. Development of models for adverse effects of radiotherapy research and patient selection is critically dependent on consistent standardized organ delineation and treatment planning for comparison of modalities.
Project description
The overall objective of this project is to instigate a national initiative for standards and automation of segmentation and treatment planning to support the development and dissemination of best practices and support national protocols for clinical research. Consistent standardized treatment planning – including organ segmentation – will serve as the necessary platform for national comparison of treatment modalities. This is particularly pertinent with the introduction of new treatment techniques in the coming years – proton therapy and MR-guided therapy.
The project is divided into two research tasks – (1) organ segmentation and (2) plan optimization.
Research task 1: Organ segmentation
Aim – Research task 1
The aim is to develop consensus national atlases for image segmentation for brain, head and neck, thorax, abdomen and the pelvic area for use in radiotherapy treatment plan generation.
Background – Research task 1
Image segmentation is inherently difficult across different RT centers due to the different interpretations of contouring guidelines. However, there are numerous benefits for multi-center collaboration, like consistent nomenclature, uniform contouring, and efficiency, which cannot be overlooked and therefore the difficult task of creating an image segmentation atlas needs to be done in a proper structure, as set up in this study.
Methods – Research task 1
For all anatomical sites the basic methodology adopted in the construction and validation of the atlases will be as follows:
- The construction of the atlases will generally be done by a collection of a total of 10-15 patients per anatomical site from all radiotherapy centers in Denmark, aiming for all patient immobilization and alignment protocol to be represented in each atlas. In addition, a diversity of patient sizes will be collected, aiming for the atlases to constitute the patient populations as well as possible. The patients should not have extensive tumor burden nor malformation from surgery so that anatomical structures are not deformed from their natural state. The organs at risk will be contoured according to the site-specific DMCG guidelines and in cooperation with the DCMG’s. The contours will be validated at all involved centers, by expert oncologists editing the contours. The reviewed contour data will be collected in the national image bank and analyzed according to agreement of volumes and surface distances between contours. For each anatomical site, the respective DMCGs will host a workshop in which the results of the review will be presented and discussed. The goal for each workshop is to finalize consensus atlas.
- The consensus atlases will be used for auto-segmentation in the different software implementations across the departments. The main part of the data in the atlases will be used for developing auto-segmentation tools, however, a smaller sub-cohort will be used for validation of the full segmentation workflow. Here the performance of the atlas will be benchmarked using recognized contouring validation metrics like similarity-index and mean surface distance etc.
- Site-specific issues for consideration:
- The brain atlas will be constructed for MR images only, and there will be limitations in which imaging sequences that they will work for.
- The hand and neck atlas have an overlap with the brain atlas, however, it will only be for CT images, which means that the processes of construction and validation are separate.
- Both the thorax and the pelvic atlases will have several treatment sites as focus (breast, esophagus, lung, prostate, cervix, etc). Not all organs as risk will have the same focus for all treatment sites, hence the atlases could be split into sub-atlases.
Research task 2: Plan optimization
Aim – Research task 2
The aim is to develop tools to support the establishment of national consensus guidelines for optimal treatment planning for brain, head&neck, lung and breast cancers.
Background – Research task 2
High plan quality is a prerequisite for good quality RT and clinical trials. However, what is high plan quality? This is not so easy to quantify in particular where there are multiple OAR and very little evidence of which OAR should be spared over others. This study will first generate metrics of plan quality, from which one can compare plans and quantify which plan has the highest plan quality, independent of radiotherapy modality. Secondly, high-quality plans will be generated for plan comparison.
Methods – Research task 2
A collection of exemplary patients will be gathered for each treatment site. These exemplary patients from all treatment sites will be sent out once every year to all participating centers, for treatment planning according to national and local guidelines and plan evaluation criteria.
Annual national workshops will be held for discussion of the resulting treatment plans with the aim of identifying best practices and incremental plan improvements and move towards consensus plan quality.
A set of metrics for plan evaluation and comparison will be developed, on which the workshop discussions can be based. This includes not only dose-volume parameters, but also complementing tools; robustness evaluation towards delineation uncertainties and geometric uncertainties, plan deliverability, and variations in dose objectives for target and organs at risk and prioritization of these. A national working group with participants from all involved centers has been established to discuss relevant metrics. All involved DMCGs will be consulted, to establish the application of the metrics for the various treatment sites.
Time trends in plan quality will be evaluated for each center, and geographical as well as time trends in differences based on plan priorities and system platform will be quantified.
Expected results
- For all three anatomical sites, a national consensus atlas will be readily available for all centers to use. The centers will be able to adopt the atlases in their workflow and gain consistency in organs at risk delineation and naming and save time in the contouring process.
- For relevant treatment sites, optimal treatment planning strategies and best practice examples will be identified. Libraries of optimal treatment plans based on various system platforms will be collected, constituting input for automated treatment planning, and for plan assessment. The centers will be able to use this to continuously evaluate and improve plan quality, and at the national level best practice can be developed and disseminated through a continuous update of optimal plan libraries
Impact/Relevance/Ethics
- The impact of the atlases will be a more uniform identification of the organs across the radiotherapy centers. This is important for the individual patient since treatment plan quality and selection of treatment modality (for instance proton vs photons) rely heavily on high-quality contours.
- Automation of the organ segmentation will be possible with the national consensus atlases and in addition, consistent nomenclature for structures will be achieved, which is a highly valued feature in relation to quality assurance for nationwide studies.
- Radiotherapy plan generation will be benchmarked across the centers, and plan comparison for proton/photon modality selection will be based on common tools including scope of measures for comparison of plan quality.
-
Carsten Brink
Professor, medical physics
Odense University Hospital![]()
-
Eva Samsøe
Head of Medical Physics, PhD
Zealand University Hospital, Næstved Sygehus![]()
-
Jimmi Søndergaard
Overlæge, PhD
Aalborg University Hospital![]()
-
Christian Rønn Hansen
Radiofysisk Laboratorium og DCPT
Odense University Hospital![]()
-
Anne Vestergaard
Hospitalsfysiker
Aarhus University Hospital![]()
-
Jesper Kallehauge
Ph.D.
Aarhus University Hospital![]()
-
Uffe Bernchou
Lektor i Medicinsk Fysik
Odense University Hospital![]()
-
Lone Hoffmann
PhD
Aarhus University Hospital![]()
-
Heidi S. Rønde
Hospitalsfysiker
Aarhus University Hospital![]()
-
Kenneth Jensen
Overlæge
Aarhus University Hospital![]()
-
Stine Korreman
Professor
Aarhus University Hospital![]()
-
Ebbe Laugaard Lorenzen
PhD
Odense University Hospital![]()
-
Laura Patricia Kaplan
Physicist, PhD
Zealand University Hospital, Næstved Sygehus![]()
-
Jintao Ren
PhD student
Aarhus University Hospital , Aarhus University![]()
-
Raul Argota Perez
PhD, medical physicist
Herlev Hospital![]()
-
Nadine Vatterodt
Cand. Scient., PhD student
Aarhus University Hospital![]()